The Science: Linkage to Care
by Nicole Johns
by Nicole Johns
March 21, 2013
Linkage to care is a hot topic these days. It sounds so simple, help newly-diagnosed people get into HIV care within 30-90 days (time period depends on who does the measuring). But like with so many other things, it isn’t always that simple. Humans are complex social creatures with needs, fears, beliefs, values, desires, and experiences. These factors play a big part in whether or not a person enters HIV care right away, or at all.
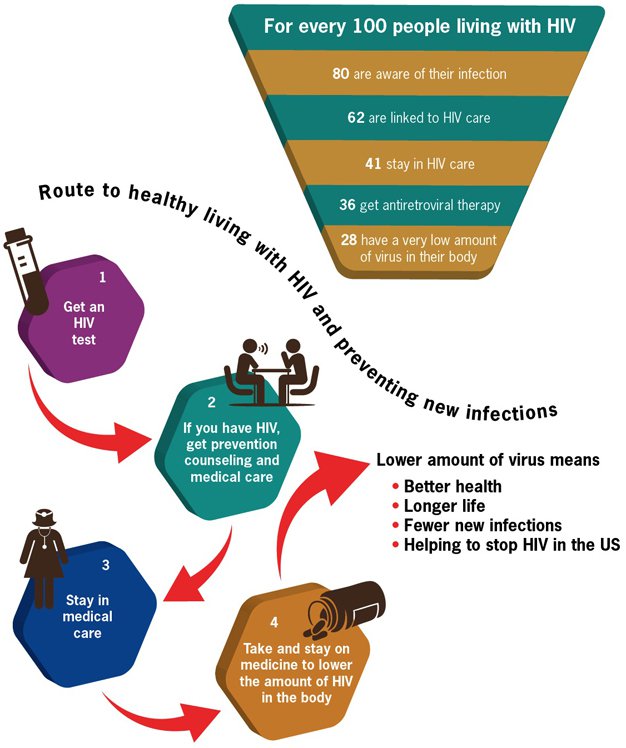
Before we go any further talking about linkage to care, we should make sure everyone understands that linkage to care is just one stop along the continuum of HIV care, as shown on the CDC’s image above and famously described by Gardner, McLees, et. al (2011). You can also check out this short Prezi to get context for the importance of linkage to care.
The CDC reports that about 80% of all people with HIV are aware of their HIV status, and only 62% are linked to care. That means that 62% of all the people in the United States who have HIV have had one HIV medical appointment. So that means 38% have not.
One way to improve our practice and service planning is to review the social science to see what researchers have found to be barriers and facilitators (things that help) to linkage. Factors vary and include individual, provider and systemic characteristics. Examples include stigma, denial, substance abuse, place of HIV testing, insurance status, health beliefs about HIV, and other socio-economic, psycho-social and provider-related concerns. Below you will find short summaries of two of the many research articles and resources related to linkage to care, followed by two more resources by Dr. Michael Mugavero (an expert on linkage and retention) to get more information.
This was a small qualitative study of patients at a clinic in Mississippi.
Barriers:
Factors that helped linkage and retention:
Social support was the factor most often mentioned by participants, because it was believed to have the biggest impact on the patient's motivation to seek appropriate care. Competing needs and responsibilities are a main reason people miss care appointments. These competing needs are particularly influential for lower income PLWHA who may not have access to resources or support to meet competing needs and attend appointments.
Study data from New York City's Medical Monitoring Project (MMP) dataset (2007 and 2008), part of the larger CDC (and partners) surveillance project and the Never in Care (NIC) study.
Of the 513 MMP participants in 2007-2008, 23% had delayed entry in to care longer than three months after diagnosis. Two independent factors of delayed entry included an earlier year of diagnosis and testing in a nonmedical setting. Of the 28 NIC participants, over half had tested positive in a nonmedical setting. The primary reasons for delayed entry into care for both NIC and MMP were denial of HIV status and not perceiving a need for medical care.
Predictors of Late Linkage to Medical Care After an New HIV Diagnosis by Michael J. Mugavero. (A part of the Medscape Education series on HIV)
eHIV Review Podcast, Vol 1, Issue 4 (Transcript)
Featured Cases: Linkage and Retention in HIV Medical Care by Dr. Michael Mugavero
This website is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of an award totaling $20,808,001. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by HRSA, HHS, or the U.S. Government. For more information, please visit HRSA.gov.