What is health equity?
by Nicole Johns
by Nicole Johns
Sept. 10, 2019
In order to understand the complexities of health equity, we need to define some terms. The goal of this post is to define these terms using simple and clear language which means nuance and complexity may be lost. This primer defines equity, health equity, social determinants of health, and health disparities. In future posts, we will dig deeper into each of those terms and look at specific examples of health disparities and social determinants of health.
In the simplest terms, equality is giving everyone the same resources. Equity is giving people what they need. See the images below for a great example. In the first picture all the people are given the same sized box to see over the fence. The first person doesn’t even need a box to see over the fence. The second person can barely see over the fence, but the third person can’t use the box because it does not accommodate their wheelchair. This first picture is an example of equality. However, the second picture shows everyone enjoying the game because they received what they needed see over the fence.
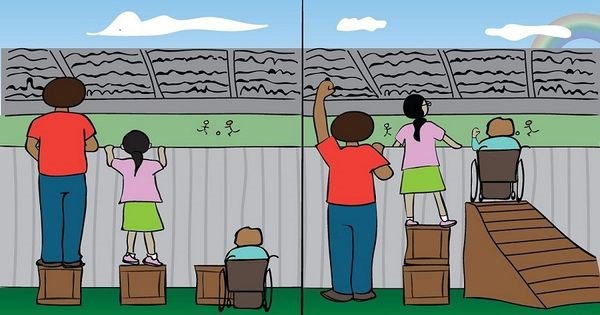
A version of the equality vs. equity picture that highlights the importance of inclusion of people with disabilities. Image courtesy Maryam Abdul-Kareem.
Health equity means that all people have a fair opportunity for health. Different groups of people will require different resources and support to maintain and promote their health. Health equity means removing obstacles to health like poverty and discrimination. Health equity means improving conditions for communities with health disparities. Health disparities exist due to discrimination and marginalization of certain groups.
Health disparities are differences in health between groups of people. Health disparities exist because of inequitable access to health-promoting resources. Societies discriminate against groups because of their identity or social status. Health disparities are not caused by personal choices, but because of society-level factors, some of which affect individual behaviors.
Racial segregation is a good example. Historic and existing policies have promoted white people’s access to mortgages, safe communities, good schools, etc. Housing discrimination is illegal, but unfair policies around mortgages and education exist. These policies limit resources in communities of people of color and promote self-segregation of white people. When we look at data for health outcomes, we see that communities with more people of color have poorer health outcomes than similar communities of mostly white people.
In order to reduce health disparities, governments and institutions can direct resources to disadvantaged communities to address social determinants of health.
Many factors outside our control affect our health. Conditions in the places where we live, learn, work, and play affect our health. These conditions are known as social determinants of health. Social, psychological, and economic factors are strong predictors of lifetime health and well-being. Our early life experiences affect our health over our lifetimes. Some examples of social determinants of health are educational attainment, employment status, air quality, experiences of violence, housing security, mass incarceration, HIV stigma, and quality of personal relationships.
Governments, institutions, and communities can make decisions that promote and protect the health of the people. Health equity is the principle, or value, to eliminate health disparities. We monitor our efforts towards health equity by measuring the change in outcomes among disadvantaged groups and the differences in health outcomes between disadvantaged groups and advantaged groups.
Health disparities are not inevitable. Health equity is possible but only by improving the social determinants of health of disadvantaged communities.
The Robert Wood Johnson Foundation published a report on Health Equity and a webinar about building health equity in 2017.
3 min video on health equity from The Health Equity Institute
The Office of HIV Planning has a presentation about Social Determinants and HIV.
The Philadelphia EMA’s Integrated HIV Prevention and Care Plan outlines the EMA’s plans to address social determinants of health of those living with, and at risk for, HIV.
This website is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of an award totaling $20,808,001. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by HRSA, HHS, or the U.S. Government. For more information, please visit HRSA.gov.